The NHS Pay Review Body is supposed to be an independent body, and in some ways it is; but in very important ways it allows itself to be steered by ministers and civil servants.
Its 35th report, for 2022, is a bundle of contradictions – offering some hard-hitting facts and revealing analysis, repeating some of the telling evidence the panel has received from trade unions and other bodies – but also being limited by the remit letter received from then Health and Social Care Secretary Sajid Javid, which set them on a mission impossible.
Javid’s remit, written on November 30 as the surge in price inflation was only just beginning, requires any increase to fit within the existing budget – yet at the same time “ensure that the NHS is able to recruit, retain and motivate its Agenda for Change workforce:”
“As the NHS budget has already been set until 2024 to 2025, it is vital that planned workforce growth is affordable and within the budgets set, particularly as there is a direct relationship between pay and staff numbers.”
Given the scale of current and projected inflation the PRB has not been able to comply completely with this brief, but they have stopped short of making the logical call for extra funding to cover the excess cost of their proposed pay increase. That’s why ministers have been willing to accept the PRB recommendations in full.
But the contradictions in this approach appear again and again. For example Chapter 3 reports warnings from England’s Department of Health and Social Care that an additional 1% of pay for the HCHS workforce as a whole costs around £900 million “which is equivalent to around 16,000 full-time nurses or 500,000 procedures.”
The PRB limply notes:
“NHS England and Improvement told us … pay awards that are higher than the affordable level, and which are not supported by additional investment, will result in difficult trade-offs during the year on staffing numbers and the ability to deliver activity volume. These decisions will have a longer-term impact on the NHS’s ability to restore services and make progress in tackling the elective care backlogs which have grown during the pandemic.”
The PRB also notes NHS England and Improvement warning that because of the scale of assumed efficiency savings built in to the Long term Plan “it would not be credible to rely on further efficiencies in order to fund headline pay awards.”
But, confined by the remit letter, the PRB does not make the obvious recommendation that to prevent potentially damaging consequences of a funding gap the government must fully fund any award.
The PRB also notes briefly in passing the huge gap between private sector average earnings growth (8.2% in the three months to March 2022) and public sector average earnings growth at 1.7% – “having fallen from a peak of 5.6% in March 2021 when parts of the public sector were working longer hours as part of the response to the COVID-19 pandemic.”
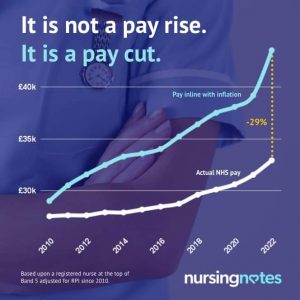
The issue of pay justice after more than a decade of falling real terms pay across the NHS also emerges in repeated warnings that the lower pay bands of Agenda for Change now offer hourly rates, shift patterns, stressful and demanding work and limited flexibility of working patterns that compare poorly with the six largest supermarkets all offering at least £10 per hour, Amazon warehouse staff and other private sector employers also competing for staff: “Manchester Airport and Stansted Airport advertising entry level Security Officer roles starting at £12.04 p/h and £14.00 p/h, respectively.”
The PRB points out “This is compared to Band 2 roles in the NHS which are being advertised with a starting salary of £9.65 p/h, Band 3 roles at £10.40 p/h and Band 4 roles at £11.53 p/h.
“Social care providers are also experiencing the same challenges.”
To make matters worse, “the results from the 2021 Staff Survey for England are clearly worse than those for 2020, and in many instances the least positive since 2017.”
Since the 2020 Staff Survey, the proportion of staff satisfied with pay has fallen from 36.7% to 32.7%, the proportion of staff who felt that there were enough staff has reduced from 38.4% to 27.2% and the proportion of staff thinking about leaving has risen from 26.5% to 31.1%.
And stress and bullying at work are clearly factors in the most common causes of sickness absence now being “anxiety, stress, depression and other psychiatric problems.”
Interestingly the PRB does not buy in to the Tory mythology that seeks to blame inflation on high wages, noting that drivers of the highest recorded level of inflation for 40 years include “increases in the costs of consumer goods, underpinned by strong demand from consumers and supply chain bottlenecks …” while “another important driver of inflation is energy prices.”
Ministers will not have been too pleased to read, albeit tucked away in the PRB report:
“We note the concerns that increases in pay could feed into a wage-price spiral, although also recognise there are other fundamental drivers of current inflation challenges. As earnings growth remains substantially below inflation, we judge that increases in earnings present a much lower risk to increasing the rate of inflation compared to some of the other fundamental drivers.”
However the pressures are not only being felt on the lower pay bands: the PRB emphasises the need to “retain the expertise of senior healthcare professionals, primarily at Band 6 and 7, who will be instrumental in supporting … new trainees and recruits.”
But this quite proper concern is not reflected in the recommendation of a flat rate £1,400 increase, which gives these more senior staff an increase of less than 4%. While Band 6 and 7 staff will have their £1,400 award “enhanced” to guarantee a 4 per cent uplift, they have already endured years of below inflation pay increases, and if the award is not increased they will face even more.
Further up the pay scale the award is even more tight-fisted, meaning the increase drops to between 2.6 and 1.5 per cent for managers on band 8, and 1.3 per cent at the top of band 9.
The PRB admits that its recommendations have to combat more staff leaving the NHS: “After reduced levels of attrition during the COVID-19 pandemic, we are now seeing leaver rates returning to pre-pandemic levels and, in some cases, leaver rates are returning to levels last seen before the three-year AfC deal in 2018. … Year-on-year falls in the
number of midwives are being seen for the first since NHS Digital began publishing leaver data in 2009.”
The PRB admits “there are substantive workforce risks related to recruitment, retention, motivation and morale. The NHS is expected, post-pandemic, to deliver increased service levels as part of the elective recovery plan. Many staff have not yet had the chance to recover from the COVID-19 pandemic. We are aware of the mental health and wellbeing support measures that have been put in place, but we heard consistently in evidence and on our visits that staff do not have the time or space to access the services in place.”
The private health sector is also eager to poach more NHS trained staff as more people pay to jump growing waiting lists: “Whilst rates of base pay in this sector are comparable, it is widely acknowledged by all parties that in the private sector working pressures are significantly less and there are increased opportunities for flexible working.”
While they are “aware that the NHS is operating within a heavily constrained budget envelope,” the PRB argues: “However, it is necessary to increase the investment in staff pay to go some way to reduce the risk that pay is a reason to leave NHS service; to protect the service from additional temporary workforce costs; and to protect risks to patient care from the impact of increased vacancies and an overstretched workforce.”
But after all of the common sense and evidence, the PRB’s conclusion is a recommendation that as Jaimie Kaffash, editor of GP magazine Pulse sums up as “both too much and not enough”. It’s more than the NHS is funded to pay out, and already questions are being asked about where the axe will fall in order to bridge even the £1.8bn additional costs of the PRB award: but it’s not enough even for the lowest pay bands to match projected inflation.
As the unions take note of the widespread anger at an award that falls so far below this year’s predicted level of inflation, and begin to consult and prepare for ballots on industrial action they will be able to draw on some of the arguments and information in the PRB report.
But they will need more courage and conviction than the PRB panel if they are to wage action powerful enough to force the government to increase not only the pay award, but also the funding of the NHS to ensure that any further increase is not at the expense of patient care, safety and the rebuilding of services after the pandemic.
The PRB report makes repeated reference to the need to recruit and retain staff if the NHS is to stand any chance of containing and reducing the waiting list, which has risen to 6.6m since the report was written.
The sheer scale of the waiting list and its likely upward trajectory until at least 2024 is described at several points in the report, perhaps most remarkably in the evidence from NHS Employers (p156).
They recognise “tension in budgets, alongside also recognising the inefficiency of high levels of funding that goes into contracting agency staff where there are workforce gaps.”
According to NHS Employers “the NHS has the longest waiting lists ever recorded, with 1 in 6 people [over 9 million] expected to be on waiting lists in 18 months.” They warn that “it is critical that the NHS attracts more staff with increased pay so a higher volume of patients can be treated.”
It appears that they don’t say so, but of course NHS Employers are also aware that without additional funding to cover the costs of the pay increases there is no guarantee that more patients can be treated or services maintained.
Dear Reader,
If you like our content please support our campaigning journalism to protect health care for all.
Our goal is to inform people, hold our politicians to account and help to build change through evidence based ideas.
Everyone should have access to comprehensive healthcare, but our NHS needs support. You can help us to continue to counter bad policy, battle neglect of the NHS and correct dangerous mis-infomation.
Supporters of the NHS are crucial in sustaining our health service and with your help we will be able to engage more people in securing its future.
Please donate to help support our campaigning NHS research and journalism.


