1. Healthcare costs are rising with need
The key idea of the NHS is to share healthcare costs fairly across society, not pass them onto the individual. Compelling evidence supports the need for annual funding rises of 3-4% over the next decade. Back in 2018 the Institute of Financial Studies calculated that the NHS will need an extra 3.3% in funding a year for the next 15 years just to keep pace with cost pressures.
These rises were calculated (but not consistently implemented) to help the NHS cope with the rising numbers of older people, those living with chronic disease and the cost of medical advances – all factors which health economists can include in their modelling. But this figure takes no account of the extra costs from the pandemic or the impact of higher-than-expected prices.
2. Inflation means planned spending will fall in 23/24
According to the Health Foundation: planned total health care spending will increase by £3.1bn (1.7%) in 2023/24, and £4.9bn (2.6%) in 2024/25 in cash terms, but adjusting for inflation, planned total health care spending will decrease by £1.5bn (-0.8%) in 2023/24, and increase again in real terms by £1.9bn (1.0%) in 2024/25.
This figure falls well short of the 3.6% average annual rise given to the NHS since its launch in 1948.
3. Aggressive efficiency drives and overly optimistic gains from technology
Over the last decade governments have consistently factored excessive efficiency gains into their funding packages. Historically, the NHS has achieved efficiency gains of around 1% a year – more than in the wider industrial sector, however governments have frequently called for levels of 2-4%. In reality NHS managers can only achieve these by cutting services or avoiding expenditure.
4. Longterm funding is needed to solve the workforce crisis
Lack of NHS capacity lies at the heart of the problems with NHS waiting lists. It has also created the work pressure that is driving staff away from the NHS. The government has announced a much-needed expansion in training places, part of a plan originally promised in 2017. Although welcome, commentators are calling for urgent clarity around what funding will arrive and when, and how long-term this commitment will be.
5. Resolution of all pay disputes
Current budgets do not include a settlement for all outstanding NHS pay disputes. Establishing a situation in which the NHS understands the it financial outlook is an essential component in building a sustainability, tackling waiting lists and retaining staff.
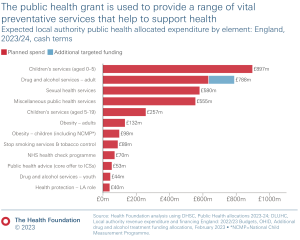
6. Invest in prevention now and it will help to control future health costs
Public health budgets have been cut by 24% on a real-terms per person basis since 2015/16. Health authorities have cut funded programmes around smoking, alcohol and diet. The NHS spends around 10% of its budget on treating diabetes – and 80% of that goes on the complications from the disease. Huge gains in health and reduction in health expenditure are possible with investment in sickness prevention.
In a Diabetes UK survey of 10,000 people with diabetes, “1 in 3 respondents had no contact with their diabetes healthcare team in 2021. Workforce shortages are a major driver of this disruption.
7. Strong financial pressures are already evident across the NHS
This pressure is already affecting local decisions about what services can be afforded and raising the likelihood of cuts. Two thirds of the Integrated Care Services (local NHS commissioners) are already facing a £1.3bn deficits. Whilst hospital trusts are on course for a combined deficit of £2bn.
8. The cost of delayed maintenance and repairs to England’s hospitals has rocketed
The backlog in hospital repairs has risen from £6bn in 2019 to £10.2bn in 2022, Half a dozen hospitals were built in the 1970s with defective concrete planks that are now a structural threat. Over the last decade capital cash strapped hospitals consistently reallocated capital funding to meet the day to day running costs in the NHS, the recent increase of 0.2% in real terms is therefore insufficient to meet the size of the backlog.
9. A decade of underinvestment
Average health spending in the UK between 2010 and 2019 was £3,005 per person – 18% below the EU14 average of £3,655. Matching the spending per head of France or Germany would have meant an extra £40bn and £73bn (21% to 39% increase respectively) available to spend on UK healthcare. Even though UK spending has equalled the EU average, spending per head of population, is still significantly lower than France, Germany and the Netherlands.
10. A long term plan to consistently to increase NHS funding over the next decade is crucial
A longterm plan is needed to raise NHS capacity and provide more care, and to stop relying on costly private sector solutions. This is a key (but not the only) driver to improving access and standards. Only 10% of the public think the government has the right policies on the NHS – 82% believe funding should be increased and roughly the same percentage think the NHS should be funded primarily through taxation.
Dear Reader,
If you like our content please support our campaigning journalism to protect health care for all.
Our goal is to inform people, hold our politicians to account and help to build change through evidence based ideas.
Everyone should have access to comprehensive healthcare, but our NHS needs support. You can help us to continue to counter bad policy, battle neglect of the NHS and correct dangerous mis-infomation.
Supporters of the NHS are crucial in sustaining our health service and with your help we will be able to engage more people in securing its future.
Please donate to help support our campaigning NHS research and journalism.