Ways to prevent illness get less public discussion than the state of our health care and yet these services – commonly known as public health, have a major impact on the country’s health, but with better policy from the government, they could do much more to help reduce the pressure on the NHS, improve access to healthcare and reduce health inequalities.
BACKGROUND:
Importance of public health
Public health workers were crucial to the delivery of the Covid-19 vaccine programmes and to the track and trace functions that can control the spread of all communicable disease.
In recent years changes in public health policy have affected us all. The smoking ban, the soft drinks industry levy (‘sugar levy’), minimum unit pricing on alcohol in Scotland, HPV vaccination for boys and girls, tobacco advertising bans and cancer screening improvements, have all made a substantial impact upon our health.
At the end of 2023 UK a public health research partnership delivereed The world’s largest PrEP implementation trial to eradicate new HIV infections,proving that it reduces the chnce of infection by 86%.
“Public health is essential to all aspects of health and wellbeing and is crucial to reducing health inequalities and influencing the wider determinants of health. Public health’s historic endeavours have led to enormous advances in the control of communicable disease, through immunisation, clean water and sanitation.” – Faculty of Public Health
What services?
Today, public health services provide a wide range of preventative services, including smoking cessation, drug and alcohol services, children’s health services, including health visitors and vaccination programmes, and sexual health services, as well as broader public health support across local authorities and the NHS.
Who provides public health?
The NHS provided these services for most of its 75 years, but since 2014, they have been provided primarily by local authorities but often in association with the NHS. They are funded by a grant from the Department for Health and Social Care (DHSC) budget.
ISSUES:
Health and wellbeing are now in retreat
However, in recent times the health and wellbeing of the nation seems to have taken a downturn. In November 2022, Andy Haldane, the chief executive of the Royal Society of Arts said in the Health Foundation’s REAL Challenge lecture.
“We’re in a situation for the first time, probably since the Industrial Revolution, where health and wellbeing are in retreat”.
After over a 100 years of progress, the health and well being of the British public is now going in reverse. The trend can be seen in data published by the Health Foundation on the increasing number of people aged 50-69 not working due to ill health.
The reasons for this trend are complicated, but the Health Foundation noted that although Covid-19 is a factor – due to long Covid and the backlog in health care – the problem began before the pandemic.
Life expectancy improvements are slowing
As well as the increase in long-term ill-health, from 2011 the trend to improving life expectancy has slowed in England after decades of steady improvement. Then along came Covid and life expectancy fell sharply.
One major factor in the increase in long-term ill-health among the population and the stalling in life expectancy growth, is the downgrading and underfunding of public health services over successive Conservative governments. Just as public health services were the main driver of increasing the health of the population for more than one hundred years, so reducing investment in them is having the reverse effect.
Prevention is much cheaper than cure
The public health interventions put in place by local authorities are excellent value for money.
Calculations by researchers at Cambridge University show that each additional year of good health achieved in the population by public health interventions costs £3,800, which is three to four times lower than the cost resulting from NHS interventions of £13,500.
The researchers suggest that investing in local public health programmes would generate longer and more healthy lives than equivalent spend in the NHS.
In May 2023, a study presented at the European Congress on Obesity in Dublin, showed that the NHS spent an average of £1,375 annually on morbidly obese patients with a body mass index (BMI) of more than 40. Obese patients with a BMI of 30 to 35 cost the health service an average of £979 annually, and those with a BMI between 35 and 40 cost £1,178 per year.
The study suggested that if everyone were a healthy weight the NHS would save nearly £14bn annually. It is public health services that are in a position to help people maintain a healthy weight and to save the NHS billions.
The charity ASH (Action on Smoking and Health) presented an analysis in January 2022, that found that, the cost of smoking to society is significantly higher than previous estimates. They show the cost of smoking to society totals £17.04bn for England each year. This compares to £12.5bn under the previous estimate.
The analysis found smokers are more likely than non-smokers to become ill while of working age and more likely to die while they are still of working age creating a further loss to the economy. Smokers are estimated to cost the NHS £2.4bn per year, due to their need for health and social care at a younger age than non-smokers. It is public health services that are in a position to help people give up smoking and to save the NHS billions.
NHS England’s figures show that alcohol-related admissions to hospital have grown by 17% over the last decade – in 2016/17 there were 337,000 estimated admissions – 2.1% of the total. And alcohol-related harm is estimated to cost the NHS in England £3.5 billion every year. Effective public health services come at a much lower cost than treatment by the NHS.
Yet, despite the overwhelming evidence of excellent value for money of public health interventions and their importance for a healthy population that would ultimately rely less on the NHS and contribute more to the economy, over the last 13 years the Conservative government has actively cut spending on public health and worked to reduce its ability to save lives.
Public health downgraded
An editorial in the BMJ in September 2022, highlighted how after over 10 years of Conservative government the importance of public health services has been downgraded and they have been chronically underfunded.
The editorial notes that since 2010, successive governments have “dismantled and defunded public health rather than recognising the importance of a healthy population and a robust and effective public health function.”
The central public health agency, Public Health England, has been abolished and replaced by the UK Health Security Agency, and this has dropped public health from its title. Three of the four chief medical officers in the UK are not public health doctors and local directors of public health were transferred from the NHS to local councils, authorities which have at the same time been steadily underfunded.
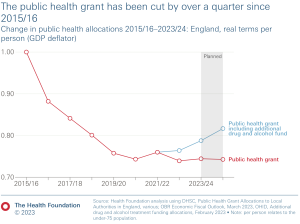
Funding down over a quarter
As well as downgrading public health within the healthcare system in England and Wales, the actual amount of funding that is provided for public health services fell by 26% from 2015/16 to 2023/24 on a real terms per person basis.
Poorest areas lose out
The cuts to funding have taken place across all local authorities, but it turns out that the areas seeing the biggest real-term per person cuts are those that are the most deprived with the poorest health outcomes – in fact those areas that are most in need of and will benefit the most from public health services.
For example Blackpool, ranked as the most deprived upper tier local authority in England, had the largest cut to its grant at £42 in real terms per person since 2015/16, according to the Health Foundation.
Back in 2019, the IPPR also found that the cuts in public health disproportionately affected the most deprived areas. When the IPPR compared the cuts in the most and least deprived ten local authorities, they found that “Almost £1 in every £7 cut from public health services has come from England’s ten most deprived communities – compared to just £1 in every £46 in the country’s ten least deprived places. The total, absolute cuts in the poorest places have thus been six times larger than in the least deprived.”
Consistent cuts
Analysis by The Health Foundation of spending from 2015/16 to 2023/24 found that some of the largest reductions in spend over the period were for stop smoking services and tobacco control, which fell by 45% in real terms, drug and alcohol services for adults down 17% and for youth down 28%, and sexual health services down 29%.
Despite a commitment in the Autumn 2021 Spending Review to maintain the public health grant in real terms until 2024/25, due to escalating inflation cuts will continue as the grant is already set to fall in real terms in 2022/23, according to analysis by The Health Foundation. There have already been severe cuts to services.
In April 2022, there was a cut of £100 million in funding for weight management services, due to be shared between the NHS and local councils, despite research showing that these services, a broad range of health advice, information and behaviour change support services, can be an effective intervention to support lasting health improvement.
Sexual health services, in particular, are struggling. Danny Beales, Head of Policy & Campaigns at National AIDS Trust, in a recent HSJ article appealed for more money for these services.
Therese Coffey’s short-lived tenure at the DHSC and Liz Truss’s as PM briefly highlighted public health services and they became the subject of headlines, as it was reported that anti-smoking and anti-obesity measures would be reversed or not put in place. Even though they are both gone, the government continues to delay important anti-obesity measures, with Rishi Sunak’s government delaying its planned ban on two-for-one junk food deals – a key anti-obesity measure – until October 2025.
Individuals and the country will suffer from under investment
The importance of public health services is clear, but all too often its vital role is ignored or downgraded by governments and much of the media. To be flippant for a moment – I don’t think anybody has pitched an idea for a long-running TV series on the day-to-day life of a public health services department somewhere in the South-West. Yet, the lives of millions of people have been saved, enhanced and extended by public health services.
Without improvements to funding, the reduction in public health services will result in missed opportunities to prevent the early deterioration of health – people who with the right interventions might have given up smoking or alcohol, will now go on to lead shorter, more unhealthy lives with all the additional negative consequences that can have for people around them and for costs to the NHS. Lack of intervention early on, leads to far more costly intervention
Individuals will suffer but also the NHS, the country and our economy will be adversely affected. If this refusal to fund public health services continues then in future a higher proportion of the country’s population will have poor health at a younger age, resulting in an increase in costs for the NHS, a fall in the number of people available to work, and the widening of health inequalities, all of which will have a negative effect across all of society and the economy.
Dear Reader,
If you like our content please support our campaigning journalism to protect health care for all.
Our goal is to inform people, hold our politicians to account and help to build change through evidence based ideas.
Everyone should have access to comprehensive healthcare, but our NHS needs support. You can help us to continue to counter bad policy, battle neglect of the NHS and correct dangerous mis-infomation.
Supporters of the NHS are crucial in sustaining our health service and with your help we will be able to engage more people in securing its future.
Please donate to help support our campaigning NHS research and journalism.