In the face of rising waiting lists government policy has aimed to increase the role of the independent sector in tackling these record delays, but as a Lowdown analysis of recent figures confirms the NHS is still shouldering the vast majority of the task.
Key points
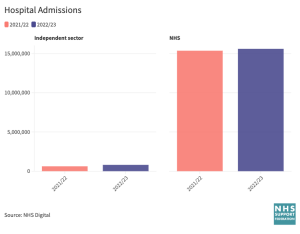
- The number of NHS hospital admissions handled by the independent sector has risen by 28% in the last year to over 800,000, but this is overshadowed by the 15.6 million admissions into NHS hospitals.
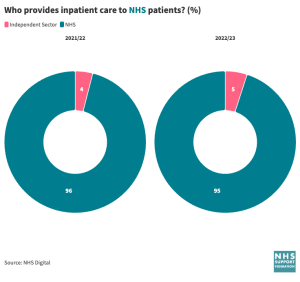
- Overall though, the share of total admissions treated by the independent sector has risen to 5%, from around 4% in 2021/22.
- The NHS continues to handle virtually all emergency admissions – 6,054,000 in the last year (2022/23).
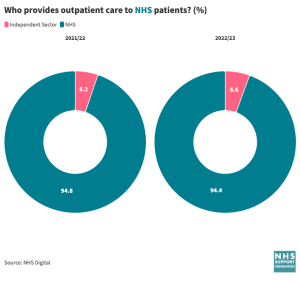
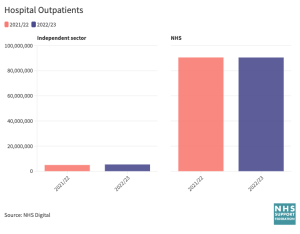
- Of the nearly 90 million outpatients attendances in 2022/3 the NHS handled just over 94%. The proportion treated by non NHS providers rose by less than 0.5%
- In the short term, private hospitals have a very limited scope to tackle the scale of the NHS waiting lists, due to limited beds, profit targets and a reliance on NHS consultants to deliver their work. A longer term policy to expand the outsourcing of NHS clinical work to the independent sector comes with considerable impacts upon the NHS and patients.
Analysis: why the plan to increase outsourcing of elective care is flawed
A central strand of the government plan to tackle growing waiting list is the expanded use of the private sector – confirmed in the NHS England’s electives recovery plan and later by its task force for implementation
Post pandemic the NHS is managing extraordinary demand and it seems reasonable that NHS patients should not suffer needlessly if appropriate alternatives can be found and funded through the NHS. However there are limits to this approach even in the short term, and in the longer term there are clear dangers for the NHS.
Reliance on NHS consultants
Operations and treatments performed in the private sector rely heavily upon NHS surgeons and doctors that are working part time in the private sector to perform them. Raising private activity will inevitably impact upon the ability of the NHS to raise its own levels of activity.
In evidence to the Commons Public Accounts Committee (PAC) last December, the Health Foundation questioned how much of the activity delivered by private providers is genuinely additional, rather than simply privatised delivery of services that NHS hospitals could have done. The PAC itself clearly agreed, and decided to write to NHS England, calling on it to write to it to explain
“the extent to which these initiatives [purchasing care from private providers] have so far generated genuinely additional activity, rather than simply displacing activity elsewhere in the NHS.”
Limited beds
In the short term, like the NHS, private hospitals have a limited bed supply, around 8000 overall. As businesses they are heavily incentivised to maximise returns by treating private patients before taking on extra NHS work.
Maximising returns
Despite the government’s desire to see more NHS patients treated in the private sector the price that private providers are paid is a stumbling block, they are lobbying to be paid more. Currently both the NHS and private sector are paid according to a fixed NHS tariff.
Fixed pricing was introduced to ensure a level playing field and ensure value for money – a rare protective measure during the era of forced competition for NHS contracts. Prior to this the inflated costs from deals struck with the independent sector treatment centres, started by the then Labour government, had incurred an average additional cost of 11.2% above NHS levels.
Inequity of access
Many of the independent hospital are sited in more affluent areas. There is considerable inequity which is embedded within the policy to expand outsourcing, and is seemingly ignored by policy makers. A Health Foundation analysis concludes,
“There is evidence of inequality in receipt of ISP-delivered care related to patient characteristics (ethnicity, deprivation, age and region). White patients are more likely to be treated by the independent sector than any other ethnicity, as are patients living in more affluent areas”
Training and standards
Cataract surgery is one area where extensive outsourcing now exists after with 46% of NHS operations being carried in the private sector, up from 11% in 2016, but serious concerns have been raised by clinicians about the impact of the policy.
In the letter, signed by nearly 200 ophthalmologists and sent to NHS England and the Royal College of Ophthalmologists and shared with The Independent, they warn of “the accelerating shift towards independent sector provision of cataract surgery” which is already having a “destabilising impact” on safe ophthalmology provision.
They predict that the wide scale use of private providers will “drain money away from patient care into private pockets as well as poaching staff trained in the NHS.” adding that “urgent action” is needed to prevent further work being given to the private sector.
Standards of patient safety in private hospitals are claimed to have improved in recent years, however CHPI and others has published material consistently raising concerns around the quality and safety of their care.
If a medical emergency happens in a private hospital, it is common for patients to be transferred to a nearby NHS hospital to access to the care and equipment they need, according to PHIN figures this affected 1 in a 1000 patients in 2021.
Transparency is developing as the attempts are made to collect wider data. Although recently the BMJ reports that,
“The Competition and Markets Authority (CMA) has given a warning to private hospitals and consultants who have made “little or no effort to comply” with their legal obligation to provide information on every episode of care they have undertaken.”
Dear Reader,
If you like our content please support our campaigning journalism to protect health care for all.
Our goal is to inform people, hold our politicians to account and help to build change through evidence based ideas.
Everyone should have access to comprehensive healthcare, but our NHS needs support. You can help us to continue to counter bad policy, battle neglect of the NHS and correct dangerous mis-infomation.
Supporters of the NHS are crucial in sustaining our health service and with your help we will be able to engage more people in securing its future.
Please donate to help support our campaigning NHS research and journalism.


