Universality
It began with one straightforward aim – to give everyone in our society access to high quality healthcare, no matter where you live and regardless of your ability to pay. For many people the NHS removed the uncertainty around being able to access healthcare during sickness.
The start of the NHS in 1948 coincided with the wider use of antibiotics making them accessible to the whole population. It had a huge impact on the management of many infectious diseases, like bronchitis and pneumonia, and in the treatment of childhood disease where before antibiotics 90% of children with bacterial meningitis died. Making medical advancements available to all remains a key strength of the NHS.
Equity and efficiency
We share the cost of the NHS fairly through the tax system, pooling the risk of ill health. Centralised funding allows for economies of scale in purchasing and ensures funding is distributed fairly. The public want to see NHS funding used wisely and waste minimised. Overall there is evidence that the NHS is already cost efficient, with less spent on administration compared with other healthcare systems that are based around charges and insurance.
Public service
The NHS has always relied upon a vast pool of committed staff, who are trained to high professional standards and are motivated by a culture of public service which prioritises the needs of patients.
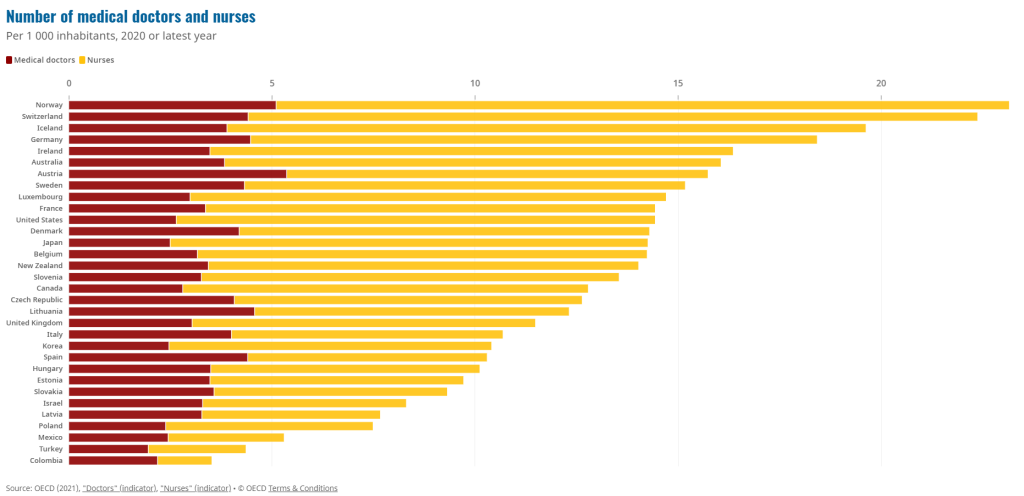
Over the last decade NHS staffing levels have not kept pace with the demand. A lack of planning and investment in workforce has coincided with a long-term rise in waiting times, which started before the pandemic. The government has published a new workforce plan but history shows that public pressure will be needed to ensure it is backed by consistent funding.
Comprehensive services
Anyone living in the UK can access a huge range of healthcare provided through the NHS, including the care of family doctors, community health services, diagnostic services, hospitals and emergency facilities. Inconsistency in funding has affected capacity and increased waiting lists, but the clinical urgency of care is an important principle in deciding priority.
A cooperative network
In 1948 the NHS replaced a patchwork of charities and local authority services with a national network that cooperates to deliver high quality services to every corner of the UK. Despite recent attempts to allow commercial approaches to be more dominant, it does not work for profit and remains largely publicly delivered.
There is some accountability to local people, but this has been reduced over recent years. However, the popularity of the NHS remains, boosted by its immense response to the pandemic, and it has a pivotal place in British society.
Active NHS supporters have regularly applied campaigning pressure on local and national politicians in order to protect and improve its services.- a cooperative network, publicly supported, that is not for profit.
Adaptive and resilient
The NHS is hugely adaptable and resilient. Over the last 75 years it has adapted to advances in technology and medicine and been hugely popular for the service it has provided. It has also had to survive through many periods of damaging reform, and cope with years of under-resourcing, proving its ability to adapt and cope under immense pressure.
Dear Reader,
If you like our content please support our campaigning journalism to protect health care for all.
Our goal is to inform people, hold our politicians to account and help to build change through evidence based ideas.
Everyone should have access to comprehensive healthcare, but our NHS needs support. You can help us to continue to counter bad policy, battle neglect of the NHS and correct dangerous mis-infomation.
Supporters of the NHS are crucial in sustaining our health service and with your help we will be able to engage more people in securing its future.
Please donate to help support our campaigning NHS research and journalism.