One in four people will experience a mental health problem each year but most go untreated. Extra funding and new approaches have been promised, but a recent Parliamentary assessment revealed that the service is still letting huge numbers of mental health patients down, why is this?
Summary:
- Staffing levels are not rising with demand – scope and standards of care falling
- Funding has been insufficient, and money has not reached patients
- Our society is not addressing the root causes of ill health, over relying on drug solutions
- Targets to treat mental health patients with same priority have been missed
- Planners of care don’t adequately involve people with a lived experience of mental health
- NHS mental health beds have been cut and services outsourced
Rising number of patients
A recent study looking at young people found a six-fold increase over the last two decades, in the proportion of 4-24 year olds who have a long-standing mental health condition.
Commenting on the Nuffield Trust research, Dr Dougal Hargreaves said “We know that there is already a growing crisis in the availability of Child and Adolescent Mental Health Services, with many more children and young people needing treatment than there are services to provide it.
The authors suggest that part of the reason for the growth in demand is the willingness to admit problems.
The evidence also shows a steady rise in mental health issues across the population as a whole.
Economic uncertainty, the influence of social media and rising expectations of life have been suggested as factors. 92% of mental health trusts said in a recent survey that changes to universal credit and benefits are increasing demand for services, as are loneliness, homelessness and wider deprivation.
The most recent figures from NHS digital (2014) shows 9.3% of the population reporting a common mental health issue.
Staff numbers have not kept up with demand
In 2013 there was 1 mental health doctor for every 186 patients accessing services. In 2018 this has fallen to 1 for every 253 patients.
The number of nurses per patient has also dropped. In 2013 there was 1 mental health nurse for every 29 of patients accessing services, by 2018 that had fallen to 1 for every 39 patients.
A survey by UNISON of staff working in mental health found that staff shortages were:
- a major factor preventing individuals from accessing services early (74 per cent)
- a reason for the increased frequency of violent incidents experienced in the past year (87 per cent)
- a reason for staff having to work unpaid overtime (57 per cent).
Last year it was reported that two thousand mental health staff a month are leaving their posts in the NHS in England, according to figures from the Department of Health and Social Care (DHSC).
10% of vacant specialist mental health posts are unfilled.
Funding is insufficient
An analysis of the most recent budget (2018) by economists at the Health Foundation noted that,
‘Extra investment in mental health services will see funding grow broadly in line with the total health budget but this will mean simply maintaining the status quo, which sees just 4 in 10 people who need it receive mental health support. To see some improvement, with provision increasing to 7 in 10, the service would need an extra £1.5bn on top of what the chancellor has announced.”
An overwhelming majority (81%) of trust leaders said they are not able to meet current demand for community CAMHS and more than half (58%) said the same for adult community mental health services; more than half (56%) could not meet demand for crisis resolution teams.
Commissioners don’t involve people with a lived experience of mental health
A report by the charity Rethink found that only 1% of clinical commissioning groups co-produce their mental heath services with users and carers, they concluded
“Decisions about complex care need to involve the people using them.” CCGs are failing to adopt co-production despite the fact that it was set out as a standard approach in the mental health strategy produced by NHS England.

Mental health is still given less priority to physical health
There is less stigma attached to mental health services, but they only received 13 per cent of the NHS budget despite the fact that mental ill health accounts for 23 per cent of the disease burden.
For three years in a row, 40 per cent of mental health trusts received a cut in their funding (2013-2016) according to research by the Kings Fund. In the last year (2017-18) 21 per cent still suffered a fall in income.
Overall, since 2012/13, funding for mental health trusts has increased by just 5.6 per cent compared to an increase of 16.8 per cent for acute hospitals.
This is despite the government have stating its commitment towards achieving parity between mental and physical health back in 2011, and has led to accusations that mental health funding is not reaching patients and according to a Nuffield Trust analysis is being diverted to cover outstanding debts.
Closure of mental health beds and other services
The number of beds for mental health patients in England has slumped by nearly 3,000 (-13%) since 2013.
Official figures show that the number of beds for those with some of the most serious conditions – including psychosis, serious depression leading to suicidal feelings and eating disorders – has fallen from 26,448 in 2009 to 18,082 in 2018.
“Cuts to services funded by local authorities also mean that preventative approaches and early intervention services are less available. Mental health leaders pointed to rising demand during winter but it is clear that these pressures on services are a year-round phenomenon.” – (NHS
Providers survey of trusts)
91% of trusts blamed council cuts as a reason for more demand for mental health services.
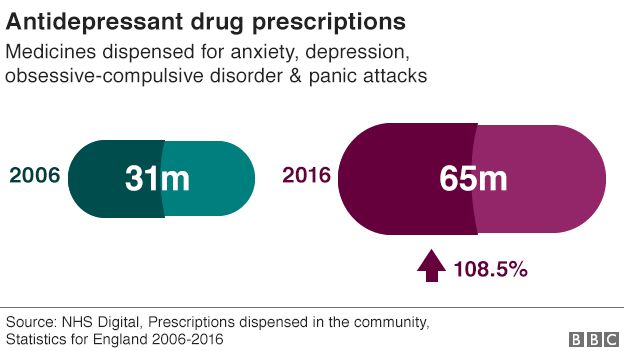
Neglecting the root causes and over relying on drug solutions
As a society we are not adequately addressing the root cause of mental health; economic uncertainty, problems with housing, social isolation, relationship breakdown and chronic disease.
More people are sleeping rough and one in five of us have mental health issues connected to housing, changes to benefits have increased suicides, a million children are living with a parent who is addicted to alcohol and two fifths of people in care homes suffer depression.
Dear Reader,
If you like our content please support our campaigning journalism to protect health care for all.
Our goal is to inform people, hold our politicians to account and help to build change through evidence based ideas.
Everyone should have access to comprehensive healthcare, but our NHS needs support. You can help us to continue to counter bad policy, battle neglect of the NHS and correct dangerous mis-infomation.
Supporters of the NHS are crucial in sustaining our health service and with your help we will be able to engage more people in securing its future.
Please donate to help support our campaigning NHS research and journalism.


