NHS England has published its much anticipated 10-year plan. It maps out a vision of improving healthcare, predicting that it will “save 500,000 lives” by focusing care on early detection and shifting money to GPs, mental health and community care.
Few commentators have knocked its ambition, but there is concern and dismay that it fails to confront what experts are calling a “national emergency” in NHS staffing.
The plan acknowledges the problem:
that “in the past decade workforce growth has not kept up with the increasing demands on the NHS”, and admits that a key part of the solution – a larger workforce budget “has yet to be set by government”.
The 10 year plan is also missing a workforce strategy – a key document that would lay out how staffing levels could change.
Consequently the plan lacks substantial proposals on staffing. Promises for more nursing and medical training places were welcomed. However, a string of charities, NHS bodies and trade unions expressed frustration at the lack of a funded strategy to deal with the staffing crisis.
Dame Donna Kinnair, General Secretary of the RCN was candid in her comments about the plan,
This is undoubtedly the right direction, yet with 40,000 nurse vacancies in England, cancer centres are struggling to recruit specialist cancer nurses, we have lost 5,000 mental health nurses since 2010, and district nurse numbers fell almost 50% in the same period….It is strange then that this plan offers no money for nurses to develop the specialisms and skills patients need.
The government has repeatedly promised to produce a NHS workforce strategy since a Lords report into the future of the NHS exposed this major fallibility nearly two years ago. Its publication has now been pushed back to later in 2019.
Hospital leaders have also been clear about what priority should be,
This plan cannot be delivered whilst trusts still have 100,000 workforce vacancies. We need urgent action to solve what trust leaders current describe as their biggest problem.”
– explained Chris Hopson of NHS Providers that represents NHS hospitals.
The government’s own auditors, the National Audit Office have published their view that NHS trusts may not be able to recruit enough new NHS staff to expand services and that some of the new funding might be swallowed up by bills for expensive agency staff.
Delays in addressing workforce issues can in part be put down to the fact that the NHS cannot fund additional staffing. This is despite the fanfare over the recent funding announcement which has been sold hard by ministers as a record uplift.
Economists analysing the government’s spending commitments have put us straight, concluding that the extra £20.5bn over the next five years is not enough to match the projected costs – barely enough to stand still but not to advance standards. The battle for the extra funds will resume in the run up to the Government Spending Review in the Autumn.
How big is the capacity crisis?
Across the NHS the number of staff vacancies is rising sharply suggesting that many trusts are finding it even harder to recruit. In the summer NHS England announced that 107,000 jobs were unfilled, including 35,000 nurse posts and nearly 10,000 doctor vacancies – enough to staff 10 large hospitals. A situation described as “dangerously” understaffed.
Some trusts are losing almost a third of staff each year. Managers are spending huge amounts of money “just to stand still” concluded a report by the Health Foundation.
International comparisons confirm that the NHS operates with very low staffing levels. The UK has the third-lowest number of doctors among 21 OECD nations, with just 2.8 per 1,000 people. It also has the sixth-smallest number of nurses for its population with just 7.9 per 1,000 people.
Growing gap between demand and supply
The staffing crisis in the NHS is deepening so fast that the service could be short of 350,000 key personnel by 2030, health experts have warned. They blame, “an incoherent approach to workforce policy at a national level, poor workforce planning, restrictive immigration policies and inadequate funding for training places”
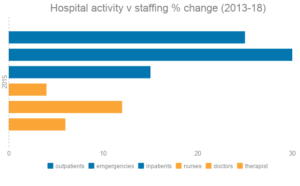
The gap between NHS staffing levels and patient demand has been growing consistently. An analysis by the NHS Support Federation shows that over the last five years the number of outpatients has risen by 24% and emergencies are up by nearly a third and yet the number of nurses in hospitals has risen by only 4%, doctors 12% and therapists 6%.
Since 2013, the number of mental health patients accessing services across England has risen by 30%, while the number of doctors has fallen by 2% and the number of mental health nurses by 1%. The number of beds for mental health patients has slumped by 13% (2,954) across England.
GP numbers have barely risen, despite a government target to recruit 5000 more. While between 2007-14 the number of patient contacts rose by 16%.
Eight years of record underfunding has left many NHS providers with persistent debt. Last year 44% per cent of trusts overspent their budget by £1bn. Many have been forced to take out expensive loans from the Department of health. It therefore remains unclear how NHS bosses will be able to set about recruiting the staff they need and retaining the teams they have.
Solutions?
In answer to the growing pressure on services the longterm plan proposes ways to reorganise and treat patients in different settings away from hospitals.
- more patients are to be treated by new community-based teams, lessening the pressure on hospitals.
- new technology will be employed to reduce the 400,000 face-to-face appointments each year in outpatients and GP practices
The shift to treatment in community has raised questions as to where the staff will come from to deliver this care. Services provided care outside hospital have already been badly affected by under funding in the NHS and cuts to social care and other councils provided services, like public health.
Between 2010 and 2016 the number of full-time equivalent qualified District Nurses in England fell by 46.4%
Caseloads have been rising for health visitors and their numbers fell to 8,497 in September last year and again to 8,016 in May this year, following cuts to the national spending on public health.
The crisis in social care has consistently piled on the pressure on other services. This is a key part of the care system and yet a decision over social care funding has been repeatedly put back by the government, frustrating charities and their supporters. The knock on effect on health services is well known, but with the stated intention of NHS longterm plan to be to integrate care services this funding question must be answered for any progress to be made.
Labour propose a national care service. “to encourage councils to explore more ethical ways of commissioning services to spur innovation, drive up quality and create a more vibrant provider sector.” Their estimated price tag is £3bn but there is little detail available about how this would boost capacity and integrate with the NHS.
One area where funding is not a problem is the recruitment of volunteers. The longterm plan also sets out an ambition to double the number of volunteers working within the NHS, with the clear implication that have a significant role to play in help the NHS to deal with demand pressures. This has drawn criticism that the NHS needs to be careful not to lean on volunteers to do the work of paid staff, with obvious implications and dangers for patient care.
There is consensus in the reaction to the Long term plan. Positive proposals and laudable ambitions to improve services are acknowledged, but these are all overshadowed by a lack of strategy and funding, on staffing, that will undermine the entire NHS plan.
UNISON head of health Sara Gorton said: “
Finding the NHS more staff, and holding on to those it already has, is key to the success of the government’s plan. The plan is honest about the scale of the staffing challenge. But nothing will happen without more money to attract new recruits and train existing employees. The government must act now, or its plan will fall at the first hurdle.
Dear Reader,
If you like our content please support our campaigning journalism to protect health care for all.
Our goal is to inform people, hold our politicians to account and help to build change through evidence based ideas.
Everyone should have access to comprehensive healthcare, but our NHS needs support. You can help us to continue to counter bad policy, battle neglect of the NHS and correct dangerous mis-infomation.
Supporters of the NHS are crucial in sustaining our health service and with your help we will be able to engage more people in securing its future.
Please donate to help support our campaigning NHS research and journalism.