For years, governments have failed to meet targets to recruit enough GPs, but now trained doctors are struggling to find posts. The reason it seems is not an excess of doctors but chronic underfunding, workforce policy decisions, and a significant lack of investment in healthcare infrastructure.
The scale of the problem is striking: a BMA survey found that 84% of locum GPs across England reported significant struggles in securing consistent employment, prompting many to reconsider their future within the NHS or even in the medical profession altogether.
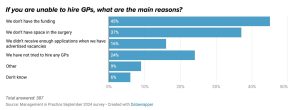
According to recent Management in Practice research, nearly half (45%) of practice managers cited funding shortages as the primary barrier to employing additional GPs, alongside inadequate practice premises (37%).
Ask locum GPs themselves, and many believe that an initiative to alleviate GP workloads by funding allied healthcare roles, including pharmacists and physician associates, has diverted crucial funds away from GP hiring.
A locum GP from Dorset told the BMA:
“I sacrificed my life for the NHS and now I can’t even find a job because GPs are being replaced by cheaper staff. I’ve explored countless options within the NHS to no avail so I’m taking up GCSE tutoring to make ends meet
The Additional Roles Reimbursement Scheme (ARRS) provides extra staff funding, but until April, it had only allowed GP practices to use this money to employ non-doctor roles. Critics argued that this undermined clinical decision-making and pressured non-GPs to work beyond their scope of practice.
is the new GP contract a solution?
Since April, the new GP contract, agreed with the BMA, has addressed some of these concerns, allowing resources to be more flexible across various patient-facing roles, including those of GPs and practice nurses.
However, significant issues remain as GPs must oversee and train many ARRS roles, which adds to the workload without funding additional supervision time. Many practices lack the physical space to accommodate more staff, even if ARRS funds are available to hire them.
Is funding still the core issue?
In the run-up to the new contract being published, the BMA made the case that funding has just not kept pace with the massive rise in workload, and the impact is widespread and urgent
GPs are leaving the profession at an alarming rate, driven by burnout, unmanageable workloads, and the pull of more attractive careers abroad. Even more concerning, many fully trained GPs remain unemployed or underemployed while communities struggle to access care.
Mismatch: GP funding Vs rising demand
Increase in Appointments: General practice staff saw 22.5% more patients in 2024 than in 2019. The number of patients registered with a GP in England increased by 5%, from 60 million in March 2020 to 63 million in March 2024.
GP funding: Since 2019, it has been cut by almost £350 million in real terms, representing a 6.9% cut to total payments made to general practice.
Funding increases
In 2025/26, the government allocated £13.176 billion to the GP contract, marking a 7.2% cash growth from the previous year, worth around 4.8 % after inflation, according to NHSE England or 4.2% if you agree with the calculations of the Local Medical Committees.
Analysis suggests that increased operational costs, such as National Insurance contributions and the National Living Wage, may absorb a substantial portion of the uplift. For instance, the BMA estimated that these changes could cost GP practices between £180–200 million nationally, taking a large chunk of the net benefit.
Just one in nine GPs and practice managers think the 2025/26 contract in England is a good deal for general practice, with most saying the uplift would not cancel out the impact of increased employer national insurance contributions, a GPonline poll has found.
Many practices continue to experience funding challenges, particularly in areas with higher levels of deprivation or rapidly growing populations.
-
A 2022 Health Foundation study showed that practices in the most deprived areas received £40–£60 less per patient than those in more affluent areas after adjusting for workload.
-
A 2023 BMJ study found patients in deprived areas waited substantially longer for GP appointments and experienced worse continuity of care.
Prospects for more funding in the upcoming Spending Review?
Looking ahead, the spending review is expected to set departmental budgets from 2026 to 2029. NHS leaders anticipate a small 2% real-term increase in day-to-day health spending, a decrease from the 3.8% uplift in 2025/26. The government’s Higher borrowing costs and limited fiscal headroom are likely government explanations
The squeeze on public finances has shifted government focus towards pushing for job cuts and setting high efficiency and productivity targets. Wes Streeting has publicly repeated that there is no more money without “major surgery” or reform, including more use of the private sector.
Capital investment
The government has announced a £102 million Primary Care Utilisation and Modernisation Fund for 2025/26 to improve primary care infrastructure and increase capacity for GPs and staff. This is the first national capital investment in general practice since 2020. However, experts believe this investment falls short of addressing the significant needs, with a report by Lord Ara Darzi estimating a £37 billion shortfall in health infrastructure necessary to meet standards.
Dear Reader,
If you like our content please support our campaigning journalism to protect health care for all.
Our goal is to inform people, hold our politicians to account and help to build change through evidence based ideas.
Everyone should have access to comprehensive healthcare, but our NHS needs support. You can help us to continue to counter bad policy, battle neglect of the NHS and correct dangerous mis-infomation.
Supporters of the NHS are crucial in sustaining our health service and with your help we will be able to engage more people in securing its future.
Please donate to help support our campaigning NHS research and journalism.


