Comment by writer and campaigner John Lister
One of the stock, unconvincing answers to those who have challenged the lack of local accountability in the new system of 42 “Integrated Care Systems” (ICSs) that will take over control of England’s NHS at the start of July has been to claim that many decisions in the larger ICS areas would be taken at more localised “place” level.
This has been a key factor in winning endorsement from the Local Government Association for a system that in reality keeps the NHS firmly in charge, but makes use of local councils to give a spurious veneer of more democratic and local involvement.
Exactly how much difference, if any, place-based organisation might make – especially when the dominant pressure is the financial constraints on ICSs and requirement to eliminate deficits, and with no place-level decision-making body, no public representation, little or no public access to the executive lead, and minimal, if any, information on potentially controversial issues in local news media – has not been explained.
But too many it will look like a sham.
As the new system, which has been put in place with the barest minimum of pretence of public involvement or consultation, sits on the launch-pad, a June 23 report by the Health Service Journal, based on research in May and June, has revealed that half of the ICBs have not even appointed the bureaucrats to lead the “places,” which are not expected to be functional until the autumn.
The HSJ calculates 39 of the 42 ICSs between them are set to establish 175 “places,” while three single-county ICSs (Gloucestershire, Lincolnshire and Somerset) have decided not to establish any more local bodies.
Each ‘place’ is supposed to have a single leader, accountable to the newly-established Integrated Care Boards (ICBs). But only 16 ICBs have chosen “some or all” of these executive leads. Of those who have been appointed: “The majority are CCG/ICB executives or local council executives, with a significant minority being NHS provider chief executives.”
Supporters of the changes have also argued that, in line with the letter of the Health and Care Act, ICBs which will have the full statutory powers and control of budgets will also have to “have regard to” the local strategy drawn up by broader Integrated Care Partnerships, (ICPs) which are supposed to link up the NHS with local government and other “partners”.
But the HSJ reveals only 21 of the 42 ICSs have so far even appointed their ICP chair: nine of these turn out to be also the ICB chair, underlining a complete lack of any independence of the ICP. Most of the rest are councillors.
So even before the new system creaks into gear it’s already embarrassingly obvious that the ICPs, non-statutory bodies with only the most tenuous and theoretical role or influence, and created as a sop to appease local Tory councillors, are a marginal, irrelevant appendage to each ICB that nobody will take seriously.
As we have consistently warned in The Lowdown, the new system of ICSs/ICBs marks a major further erosion of local public accountability, and the challenge for campaigners will be to keep track of changes and policies as they take shape at ICB level.
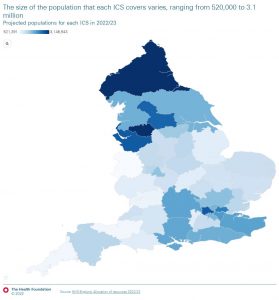
Meanwhile the Health Foundation has published a useful new study highlighting the huge variation between ICBs. It shows the range of population covered – between 500,000 and 3.1m; the varying levels of deprivation; the varying levels of potentially avoidable use of emergency and hospital care; the elective care backlog; and the near 50% variation in provision of GPs – which once again confirms the famous “inverse care law” highlighted in 1970 by Dr Julian Tudor Hart, noting that the areas with the greatest levels of deprivation consistently also had the fewest GPs per head of population, while the wealthier, healthier populations were far better provided. Even now NHS England is still only talking about this issue rather than taking any action.
Over 50 years on, with inequalities in health and in living standards widened by a decade and more of cynical government policy, a new “inverse rhetoric law” brings us more empty government words about “levelling up” the wider the gap becomes between richest and poorest.
Integrated Care Systems, established in a new wave of austerity, with Health Secretary Sajid Javid insisting that the NHS does not need and should not receive any more funding, will resolve none of this: nor indeed can ICSs address the parallel, hopeless privatised shambles of social care. And without functioning social care, the NHS cannot hope to free up the flow of patients through the hospital system.
As the new ‘reformed’ system launches as a half-arsed, chaotic, cash starved mess, under a smokescreen of unreadable and empty rhetoric, it’s up to campaigners, the unions, any local politicians who really care about their constituents and any NHS managers with a shred of self-respect to fight to expose the contradictions and gaps, challenge the short-sighted cutbacks and panic measures that are likely to follow in the autumn, and try to defend the services we all depend upon.
Dear Reader,
If you like our content please support our campaigning journalism to protect health care for all.
Our goal is to inform people, hold our politicians to account and help to build change through evidence based ideas.
Everyone should have access to comprehensive healthcare, but our NHS needs support. You can help us to continue to counter bad policy, battle neglect of the NHS and correct dangerous mis-infomation.
Supporters of the NHS are crucial in sustaining our health service and with your help we will be able to engage more people in securing its future.
Please donate to help support our campaigning NHS research and journalism.


