Nearly seven years ago the coalition government introduced the biggest ever set of changes to the NHS. Now NHS England wants to undo large parts of that legislation. The Health and Social Care Act was driven through Parliament despite a hail storm of opposition.
This week plans were published calling on the present government to introduce fresh legislation. However, this major shift in policy could be mired because the government lacks the necessary Parliamentary brawn, leaving the NHS in a dangerous hinterland.
NHS England already have skin in the game. At the start of the year they published their Long-term plan – an ambitious 10-year vision to bring councils, hospitals, GPs and non-NHS providers together, to organise healthcare in new local partnerships, breaking down all the old barriers. It was all launched with bold promises to save 500,000 lives and transform our health care.
NHS England CEO Simon Stevens knows that success rests on some critical elements that are not directly within his control. Solving the workforce crisis needs further funding and a more open immigration policy. A solution on social care has been ducked by governments for decades. A third crucial piece is the need to reorganise the NHS.
Of course, it won’t be called a reorganisation, as part of the fallout from the last NHS shake up is that the service has an understandable aversion to more change. But NHS England has already started the process, by instructing each area to form one of 42 integrated care systems (ICS) – new partnership boards made up of key organisations and providers.
The once radical ideas behind the Health and Social Care Act are being overwritten. They are at odds with NHS England’s new era of integration. NHS leaders are now trying to pull health bodies out of their competing silos, confronting the fragmentation that has predictably emerged from forced competition, but there is a problem. The laws and structures behind the market mayhem are still in place.
NHS England say they can achieve changes without Parliament, but they are clear about their preference for primary legislation and believe that “legislative change could make implementation easier and faster.”
However, the last election left the government with a majority too small for the average park kick about. Ministers know that to put new NHS legislation through Parliament would need a host of steely defenders to see off a barrage of unwelcome amendments. This explains why the promise made in the 2017 Conservative Party manifesto to put new NHS legislation before Parliament has already been quietly dropped.
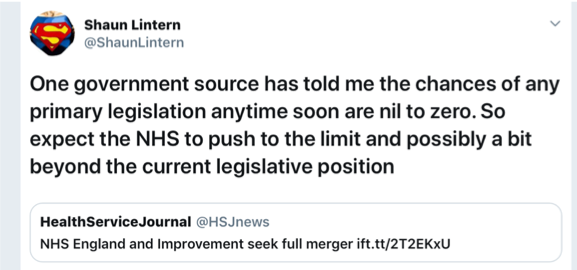
No surprise then that this week that unofficial comments reported on Twitter, from a “government source” to a well-placed journalist, appeared to firmly dismiss any prospect of new legislation.
So what’s plan B? NHS England claim that much of what they want to do can be done without legislation.
On competition, they can remove the obligation for NHS contracts to go out to tender quite easily by revoking the regulations without Parliament’s help – but the NHS is also caught by EU public contract law.
Finding a route around this largely depends on the outcome of Brexit, according to Andrew Parker a procurement specialist and partner at Hempsons. He concludes that signing a version of May’s deal would keep us under EU law for the whole of the transition period. Staying in a version of a customs union would mean that procurement rules would stay the same. No deal would separate us from EU public contract law, but that there would still be a need for other legislation to replace it.
This is a complex landscape and in bi-passing Parliament it is becoming clear that all manner of compromises, temporary patches, accountability workarounds and governance issues will emerge.
Without a change in law Clinical Commission Groups remain the lead player in terms of the current legislation, but the new integrated structures demand that they hand over control to a new local partnership board. The plan may be to give NHS foundation trusts the power to create joint committees as the basis for the 42 new integrated care systems (ICSs), but how will they work, who is in charge and how are they accountable?
John Coutts policy adviser to NHS Providers and a governance specialist has exposed some of the risks in NHS England’s Plan B.
“The partnership ‘boards’ proposed in the long-term plan to lead integrated care systems (ICSs) are not bodies corporate. They have no legal powers to make decisions and rely on delegations and committees in common to make decisions. This means that there can be no binding majority decision making which can lead to lack of clarity about when a decision has been made and by whom”
It is clear that the existing market-based structures will be stretched and pushed in ways that were not intended, and there is an unresolved legal debate amongst policy makers about how far they can go.
For all the current public disquiet with Parliament, its role in scrutinising proposed changes to complex systems like the NHS would be reassuring in this situation. The government may opt to circumvent MPs, the Lords and all their committees and process, but with that we are depriving ourselves of some our democracy’s built-in safe guards.
There is already concern that the government is abusing its powers by making changes through statutory instruments and avoiding Parliamentary discussion. The Labour leader recently launched a motion, known as a Prayer to object to this tactic being used to adjust the relationship between GPs and the new ICSs.
The need for scrutiny is also highlighted by NHS England’s plan to introduce powers that will force foundation trusts to merge. This move suggests that local democracy will once again be trumped by those at the top of the NHS. And worryingly it flies in the face of all the evidence about the success of past mergers.
Research by the University of Bristol on the impact of 102 acute hospital mergers from 1997 to 2006 found that productivity didn’t improve, waiting times increased and so did the debts of merging trusts. Similar negative conclusions were reached in a study of mergers between 2010-15 by the Kings Fund, work which also showed that improvements in care such as to stroke and cancer services have been achieved through cooperation without the need for mergers.
Campaigners will be worried that new mergers will be cover for a host of cost-driven decisions aimed at reducing debt and cutting services rather than boosting them.
In a similar vein NHS England’s plan to expand personal health budgets in the NHS needs proper public dissection. Giving patients a set sum for their care and allowing them to choose how it is spent is a high risk policy that has already been heavily criticised. What happens when the funds run out, patients will feel the pressure to top-up from their own pockets, but many will not have the means. Is this rationing by the backdoor or more charging by the front?
Equally, combining health and social care could be beneficial, but it is full of potential traps. Healthcare must remain free at the point of use and not means tested like social care. How too can we develop a new army of community-based health professionals without a commitment for them to work for NHS organisations and not in the private sector?
The implementation document from NHS England does give cheer to those who have been battling against the marketisation of the NHS. However, it also provokes concern that by not enshrining these hugely significant changes in primary legislation, controversial and flawed plans will proceed unchallenged.
It proves that to defend the NHS against damaging ideas and to promote the best, we need more democracy, transparency and accountability, not less, both at the heart of our NHS structures and in our wider society.
Dear Reader,
If you like our content please support our campaigning journalism to protect health care for all.
Our goal is to inform people, hold our politicians to account and help to build change through evidence based ideas.
Everyone should have access to comprehensive healthcare, but our NHS needs support. You can help us to continue to counter bad policy, battle neglect of the NHS and correct dangerous mis-infomation.
Supporters of the NHS are crucial in sustaining our health service and with your help we will be able to engage more people in securing its future.
Please donate to help support our campaigning NHS research and journalism.


Nearly seven years ago the coalition government introduced the biggest ever set of changes to the NHS. Now NHS England wants to undo large parts of that legislation. The Health and Social Care Act was driven through Parliament despite a hail storm of opposition.
This week plans were published calling on the present government to introduce fresh legislation. However, this major shift in policy could be mired because the government lacks the necessary Parliamentary brawn, leaving the NHS in a dangerous hinterland.
NHS England already have skin in the game. At the start of the year they published their Long-term plan – an ambitious 10-year vision to bring councils, hospitals, GPs and non-NHS providers together, to organise healthcare in new local partnerships, breaking down all the old barriers. It was all launched with bold promises to save 500,000 lives and transform our health care.
NHS England CEO Simon Stevens knows that success rests on some critical elements that are not directly within his control. Solving the workforce crisis needs further funding and a more open immigration policy. A solution on social care has been ducked by governments for decades. A third crucial piece is the need to reorganise the NHS.
Of course, it won’t be called a reorganisation, as part of the fallout from the last NHS shake up is that the service has an understandable aversion to more change. But NHS England has already started the process, by instructing each area to form one of 42 integrated care systems (ICS) – new partnership boards made up of key organisations and providers.
The once radical ideas behind the Health and Social Care Act are being overwritten. They are at odds with NHS England’s new era of integration. NHS leaders are now trying to pull health bodies out of their competing silos, confronting the fragmentation that has predictably emerged from forced competition, but there is a problem. The laws and structures behind the market mayhem are still in place.
NHS England say they can achieve changes without Parliament, but they are clear about their preference for primary legislation and believe that “legislative change could make implementation easier and faster.”
However, the last election left the government with a majority too small for the average park kick about. Ministers know that to put new NHS legislation through Parliament would need a host of steely defenders to see off a barrage of unwelcome amendments. This explains why the promise made in the 2017 Conservative Party manifesto to put new NHS legislation before Parliament has already been quietly dropped.
No surprise then that this week that unofficial comments reported on Twitter, from a “government source” to a well-placed journalist, appeared to firmly dismiss any prospect of new legislation.
So what’s plan B? NHS England claim that much of what they want to do can be done without legislation.
On competition, they can remove the obligation for NHS contracts to go out to tender quite easily by revoking the regulations without Parliament’s help – but the NHS is also caught by EU public contract law.
Finding a route around this largely depends on the outcome of Brexit, according to Andrew Parker a procurement specialist and partner at Hempsons. He concludes that signing a version of May’s deal would keep us under EU law for the whole of the transition period. Staying in a version of a customs union would mean that procurement rules would stay the same. No deal would separate us from EU public contract law, but that there would still be a need for other legislation to replace it.
This is a complex landscape and in bi-passing Parliament it is becoming clear that all manner of compromises, temporary patches, accountability workarounds and governance issues will emerge.
Without a change in law Clinical Commission Groups remain the lead player in terms of the current legislation, but the new integrated structures demand that they hand over control to a new local partnership board. The plan may be to give NHS foundation trusts the power to create joint committees as the basis for the 42 new integrated care systems (ICSs), but how will they work, who is in charge and how are they accountable?
John Coutts policy adviser to NHS Providers and a governance specialist has exposed some of the risks in NHS England’s Plan B.
“The partnership ‘boards’ proposed in the long-term plan to lead integrated care systems (ICSs) are not bodies corporate. They have no legal powers to make decisions and rely on delegations and committees in common to make decisions. This means that there can be no binding majority decision making which can lead to lack of clarity about when a decision has been made and by whom”
It is clear that the existing market-based structures will be stretched and pushed in ways that were not intended, and there is an unresolved legal debate amongst policy makers about how far they can go.
For all the current public disquiet with Parliament, its role in scrutinising proposed changes to complex systems like the NHS would be reassuring in this situation. The government may opt to circumvent MPs, the Lords and all their committees and process, but with that we are depriving ourselves of some our democracy’s built-in safe guards.
There is already concern that the government is abusing its powers by making changes through statutory instruments and avoiding Parliamentary discussion. The Labour leader recently launched a motion, known as a Prayer to object to this tactic being used to adjust the relationship between GPs and the new ICSs.
The need for scrutiny is also highlighted by NHS England’s plan to introduce powers that will force foundation trusts to merge. This move suggests that local democracy will once again be trumped by those at the top of the NHS. And worryingly it flies in the face of all the evidence about the success of past mergers.
Research by the University of Bristol on the impact of 102 acute hospital mergers from 1997 to 2006 found that productivity didn’t improve, waiting times increased and so did the debts of merging trusts. Similar negative conclusions were reached in a study of mergers between 2010-15 by the Kings Fund, work which also showed that improvements in care such as to stroke and cancer services have been achieved through cooperation without the need for mergers.
Campaigners will be worried that new mergers will be cover for a host of cost-driven decisions aimed at reducing debt and cutting services rather than boosting them.
In a similar vein NHS England’s plan to expand personal health budgets in the NHS needs proper public dissection. Giving patients a set sum for their care and allowing them to choose how it is spent is a high risk policy that has already been heavily criticised. What happens when the funds run out, patients will feel the pressure to top-up from their own pockets, but many will not have the means. Is this rationing by the backdoor or more charging by the front?
Equally, combining health and social care could be beneficial, but it is full of potential traps. Healthcare must remain free at the point of use and not means tested like social care. How too can we develop a new army of community-based health professionals without a commitment for them to work for NHS organisations and not in the private sector?
The implementation document from NHS England does give cheer to those who have been battling against the marketisation of the NHS. However, it also provokes concern that by not enshrining these hugely significant changes in primary legislation, controversial and flawed plans will proceed unchallenged.
It proves that to defend the NHS against damaging ideas and to promote the best, we need more democracy, transparency and accountability, not less, both at the heart of our NHS structures and in our wider society.
Dear Reader,
If you like our content please support our campaigning journalism to protect health care for all.
Our goal is to inform people, hold our politicians to account and help to build change through evidence based ideas.
Everyone should have access to comprehensive healthcare, but our NHS needs support. You can help us to continue to counter bad policy, battle neglect of the NHS and correct dangerous mis-infomation.
Supporters of the NHS are crucial in sustaining our health service and with your help we will be able to engage more people in securing its future.
Please donate to help support our campaigning NHS research and journalism.
director of the NHS Support Federation
Related Posts
Ten Year Plan – A tour of the dead ends
Labour and private sector: an unequal marriage
Streeting dredges up failed policies from 2000s
Newly qualifying nurses and midwives fearful they won’t find jobs
Urgent and Emergency Care: when is a plan not a plan?
Explainer: NHS funding after the spending review