Key points
From 1 July new Integrated Care Systems will replace the existing local commissioners for health (CCGs) and take on some extra functions. ICSs will cover larger areas (42) and have capped budgets, but almost all are starting with deficits.
ICS boards contain representatives from hospitals, local authorities, GPs, community health and ambulances with the idea of improving cooperation around the planning and delivery of services.
The private sector are involved but not at board level, and concerns over funding, inequity in access between areas and the scope for future private sector involvement are still being voiced.
What is meant by Integrated Care?
Integrated care is a concept which encourages organisations to work together under a single plan. It can involve sharing budgets and merging functions, but it is not a new concept and many countries have been experimenting with it in their healthcare systems.
The plan for England is the integration of healthcare and social care organisations in order to provide a more efficient way of providing services.
There are numerous organisations involved that will have to work together. Within the NHS there are GPs, ambulance services, hospital services, and community healthcare, which will now have to work with social care and local authorities. The development of integrated care will have to involve integration within the health service itself and integration between health and social care.
Integration will also have to work with different forms of funding. The NHS services are generally free at the point of use and funded by taxation, whereas social care services are often means tested with considerable input from the individual.
This Q&A deals with England, however there are changes ongoing in Scotland, Wales and Northern Ireland. In Scotland plans are underway to establish a National Care Service that would see changes to transfer existing Integration Authorities into new Community Health and Social Care Boards. Changes are also planned in Northern Ireland and Wales to increase health and social care integration.
The NHS has been working on various forms of integration within certain geographical areas for many years. However, since the publication of the NHS ten-year long-term plan in January 2019, the development of integrated care has become a top priority.
How are the ICS organised?
By April 2021, England had been divided into 42 Integrated Care Systems (ICS). These are areas of varying size and population levels.
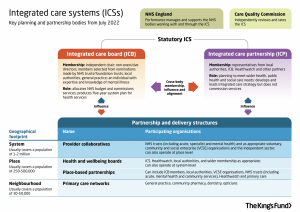
Under the Health & Care Bill that finally became law in May 2022, ICSs will become legal entities on 1 July 2022, with the creation of two related entities for each ICS – an integrated care board (ICB) and integrated care partnership (ICP). These two bodies will lead an ICS and have responsibilities within the ICS, as follows:
Integrated Care Board (ICB): a statutory NHS organisation responsible for developing a plan for meeting the health needs of the population, managing the NHS budget and arranging for the provision of health services in the ICS area. ICBs will take over the commissioning responsibilities of clinical commissioning groups (CCGs) and these will be abolished. CCG staff are expected to transfer to the ICB.
Integrated Care Partnership (ICP): this organisation will be responsible for bringing together a wider set of organisations to promote partnership arrangements and develop a plan to address the broader health, public health and social care needs of the population. Membership of the Partnership Board will include representatives from the ICB, and others to be determined locally, such as local government, NHS organisations, social care providers, housing providers, independent sector providers, and local Healthwatch organisations. They will be responsible for developing an integrated care strategy, which sets out how the wider health needs of the local population will be met.
In addition, as ICS areas are massive, often covering over 1 million people, NHS England expects these areas to be broken down into smaller units within which providers and commissioners will integrate care. It has proposed places and neighbourhoods in its guidance on ICSs.
Place-based partnerships (populations of around 250,000 to 500,000 people): served by a set of health and care providers in a town or district, connecting PCNs (see below) to broader services, including those provided by local councils, community hospitals or voluntary organisations.
Neighbourhood/Primary Care Networks (PCNs) (populations of around 30,000 to 50,000 people): served by groups of GP practices working with NHS community services, social care and other providers.
There is a considerable amount of variation in the terminology used within an ICS for these partnerships within the smaller areas of the ICS.
How will providers work within ICS?
NHS Providers are expected to join provider collaboratives. These will vary in their scale and scope.
Provider collaboratives can be ‘vertical’ collaboratives involving local acute, primary, community, social care and mental health providers, while others could be ‘horizontal’ collaboratives involving providers working together across a wide geography with other similar organisations.
All NHS providers will need to join a provider collaborative, and individual providers may be involved in more than one.
Private providers will be expected to be part of provider collaboratives, but after much campaigning, no private company will be allowed to have a representative seat on an ICS board.
The model of care provision in an ICS could involve an integrated care provider contract (ICPC), under which there will be a contract with a single organisation for the majority of health and care services in the area. The ICPC holder would be responsible for the provision of services, but may not necessarily deliver all the services itself. It could instead hold sub-contracts with other providers.
What legislation was needed for ICS?
In February 2021, the Department of Health and Social Care published the White Paper Integration and innovation: working together to improve health and social care for all, which sets out legislative proposals for a health and care bill. The white paper contained proposals to get rid of the competition rules introduced in the 2012 Health & Social Care Bill which led to an increase in outsourcing.
The proposals also include a range of measures intended to support integration and collaboration. At the heart of the changes was a proposal to establish ICSs as statutory bodies in all parts of England.
In May 2022 the Health & Care Bill had progressed through Parliament, with some amendments, and was given royal assent. ICSs will become statutory bodies from 1 July 2022.
How well developed are ICS?
Prior to the Government’s Health and Care Act passed in May 2022, ICSs had been developing in an informal way based on alliances. Despite statutory status beginning 1 July 2022, it is still unclear just how much integration has actually taken place.
Recruitment of chief executives for Integrated Care Boards (ICBs) has been slow and difficult. By December 2021 all ICS had announced their CEOs and six had confirmed that they had failed to find one.
In May 2022, an investigation by the HSJ found that most ICS had not appointed a procurement lead despite NHS England directing the new local bodies to have a dedicated director in place by April 2022. Only 12 of the 34 ICSs which responded to HSJ’s survey said they had appointed a dedicated procurement lead.
Will private companies be involved in ICSs?
The simple answer is yes, but not at the level of influence that was feared at first.
When the Health & Care Bill 2022 began its passage through Parliament, campaigners highlighted the possibility of private providers having a seat on ICS boards and thus an influence over commissioning.
After vigorous campaigning by organisations and amendments tabled by the Labour Party for changes to the Health & Care Bill so that private companies could not have representatives on Integrated Care Boards, eventually in September 2021 Health Minister Edward Argar agreed to table a government amendment to the Health and Care Bill that would prevent private interests from being on any Integrated Care Board.
The final Health & Care Bill does not allow the participation of the private sector in commissioning services and the new procurement system will allow the NHS as preferred provider, and will not permit contracts to be awarded to private providers without a proper open and transparent process.
However, outside of the Health & Care Bill 2022, there has been a major push for the use of the private sector to help reduce waiting lists for both diagnostic tests and elective surgery. NHS England’s ‘Delivery Plan,’ to enable the recovery of acute services from the after-effects of the pandemic, mentions the need for reliance on the “capacity” of the private sector extensively.
Numerous amounts of guidance, such as that on virtual wards, have been issued by NHS England reminding NHS commissioners that the private sector is there to partner with.
How will ICS funding be organised?
It was not clear in the long-term plan, published in January 2019, how funding for integrated care systems will be organised. The Covid-19 pandemic disrupted the development of ICSs as funding was increased to cope with Covid pressures.
By 2022, it was clear that funding for ICSs will be under a stricter regime than the previous two years. Each ICS has been allocated a budget and every ICS, including those that carried huge deficits going into the pandemic, will be told to deliver financial balance in 2022-23, according to draft guidance seen by HSJ.
Some ICS went into the pandemic with deficits of more than £100m, and are likely to struggle to reach a balanced position. It is unclear what the consequences will be for an ICS that fails to meet the instructions to break-even and over-spends.
Will ICS lead to rationing?
In other areas of the world, Accountable Care Organisations, which are very similar to ICS, operate with a capitated or fixed annual budget that allows the providers to retain and share any savings made. If this approach is taken for ICSs, there are concerns that services will be rationed either because the budget provided is just not enough to provide all universal healthcare services or, and this is particularly pertinent if the contract holder is a private company, to produce savings to increase the amount of budget that the providers can retain as profit.
The funding allocation for each ICS was published by NHS England in early April 2022. NHS England expects every ICS, including those who went into the pandemic with huge deficits of over £100m, to deliver financial balance in 2022-23. The ICS are being asked to hit an average efficiency target of 4% and break-even, at the same time as meeting targets for boosting elective activity and diagnostics activity.
For 2022-23 it has been reported in the HSJ that there are significant gaps between allocated and projected spending.
In late April 2022, an analysis by HSJ found that every ICS has seen its core recurrent funding reduce in real terms in 2022-23. As public sector inflation is officially forecast to be 4% this year, this wipes out the 3.3% cash increase in the funding allocated to ICS. If inflation ends up higher than this, as predicted, then the funding reduction will be greater.
NHS Providers has warned that such restrictive funding means could force NHS trusts to close services in some areas and ‘streamline’ them to single sites. There could also be an increase in thresholds for treatment, particularly in mental health, which is effectively a way of rationing care.
Dear Reader,
If you like our content please support our campaigning journalism to protect health care for all.
Our goal is to inform people, hold our politicians to account and help to build change through evidence based ideas.
Everyone should have access to comprehensive healthcare, but our NHS needs support. You can help us to continue to counter bad policy, battle neglect of the NHS and correct dangerous mis-infomation.
Supporters of the NHS are crucial in sustaining our health service and with your help we will be able to engage more people in securing its future.
Please donate to help support our campaigning NHS research and journalism.