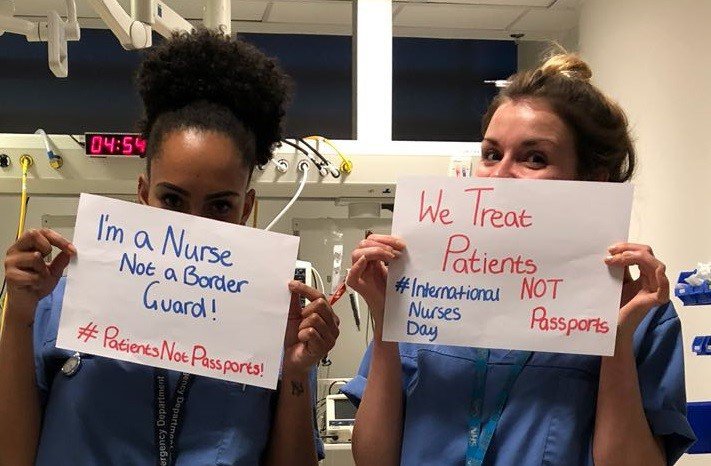
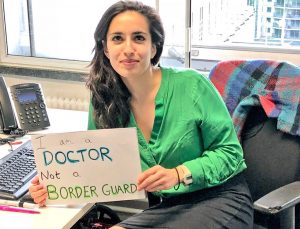
Over the last two years, the once secret scandal of NHS charges for anyone unable to prove their entitlement to free care has provoked a storm of opposition from health workers unwilling to police the ‘hostile environment’.
Keep Our NHS Public groups are working alongside campaigners from “Docs Not Cops”, “Patients Not Passports”, Medact, and Maternity Action.
The charges, broadly aimed at migrants but also affecting the Windrush generation, damage individual and public health. As the thin end of the wedge, they threaten wider charges for NHS treatment. They undermine the principle of universal health care, and contradict the NHS Constitution, medical and nursing ethics, and the responsibilities of all NHS staff to protect confidential information.
Instructing clinical and admin staff to act as border guards, places them in impossible contradictions and makes health workers unintentionally complicit with a policy that many feel is racist, and which may widen with Brexit.
GREG DROPKIN gives an extended overview of the problem and the campaigning around the issue.
Save Lewisham Hospital campaigners questioned Lewisham and Greenwich Trust over a Guardian report on the use of bailiffs to chase NHS patient debt. The Director of Midwifery and a consultant midwife expressed support, and were already auditing maternity outcomes.
The Deputy Finance Director mentioned MESH, the
Message Exchange for Social Care and Health.
Campaigners were shocked to learn that the details of suspected “overseas visitors” are passed to the Home Office through MESH, even in batches of 5000 booked for outpatient clinics. The Home Office also contacts the Trust, telling them to charge people they suspect may have had care there.

The Trust claimed to avoid racial profiling via “objective” methods developed by personal credit checking company Experian, who share data with Trusts who then focus on those without credit history.
As the Health Service Journal reported, NHS Improvement, which oversees all NHS Trusts, began a pilot to extend the scheme without checking its legality, let alone morality.
NHSI emailed 51 Trusts explaining the aim to “refine a system that can conduct bulk residency checks on all admissions and referrals in secondary care”, and to establish whether “this is an economically viable solution for use in all Trusts”.
NHSI did not assess the impact on data protection:
“NHS Improvement has not reviewed Experian’s processes and data sharing agreements for compliance either with GDPR or Caldicott principles.” It advised Trusts to take their own legal advice.
Experian developed this system in partnership with Lewisham by 2015. The Trust now plans an
independent inquiry. The campaign may propose Terms of Reference.
Many Trusts use the NHS England Pre-Attendance Form template. Patients sign their agreement to a Declaration which begins:
“This hospital may need to ask the Home Office to confirm your immigration status to help us decide if you are eligible for free NHS hospital treatment. In this case, your personal, non-clinical information will be sent to the Home Office.
“The information provided may be used and retained by the Home Office for its functions, which include enforcing immigration controls overseas, at the ports of entry and within the UK.
“The Home Office may also share this information with other law enforcement and authorised debt recovery agencies for purposes including national security, investigation and prosecution of crime, and collection of fines and civil penalties.
“If you are chargeable but fail to pay for NHS treatment for which you have be en billed, it may result in a future immigration application to enter or remain in the UK being denied. Necessary (non-clinical) personal information may be passed via the Department of Health to the Home Office for this purpose.”
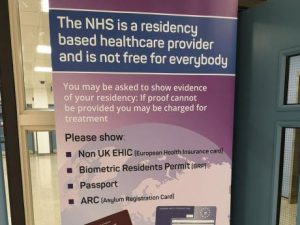 In law, NHS Trusts must determine if a patient is chargeable, but need not pursue national security, crime, fines or civil penalties.
In law, NHS Trusts must determine if a patient is chargeable, but need not pursue national security, crime, fines or civil penalties.
The Pre-Attendance Form is a generalized fishing expedition which directly contradicts Caldicott Principles of information governance which apply to all NHS staff. For example:
“Principle 2 – Don’t use personal confidential data unless it is absolutely necessary
“Personal confidential data items should not be included unless it is essential for the specified purpose(s) of that flow. The need for patients to be identified should be considered at each stage of satisfying the purpose(s).”
In March 2017, Public Health England wrote to the Health Select Committee (see pp 18-26) with evidence that sharing data externally acts as a deterrent to patients seeking healthcare:
“Effective communicable disease control requires easy and early access to clinical investigations, screening, diagnostic testing, treatment and preventative measures.
“Patients provide information to healthcare providers with explicit assurances about confidentiality and this is the basis for unfettered sharing of demographic and personal health data by patients with health systems.
“If patients have concerns that their personal information, even simple identifiers, could be shared with law enforcement or immigration enforcement agencies for the purposes of pursuing them for actual or alleged breaches of law or immigration rules, then this risks creating a real barrier to their engagement…”
Maternity
Last year, Maternity Action published “What Price Safe Motherhood?” based
on anonymous interviews by Rayah Feldman with undocumented migrant women, about their experiences with maternity care. Many were victims of abusive relationships with men, compounded by the hostile environment.
“Natasha” overstayed her student visa and was deserted by her partner when she became pregnant. After her miscarriage, Natasha received an invoice for £4,900, a letter requesting payment within 7 days, and a letter from a Debt Collection Agency.
As a result, she was afraid to go back for a check-up or to find out what had caused this miscarriage or a previous one.
“My baby was buried and I couldn’t even go. I was just so scared they were going to come and detain me. I went to see my GP, I was still bleeding then. They had to take me to the
theatre to do a D&C. I haven’t had any examination to see if it is all OK.
“At times my period is so painful, I feel cramps when I sit down, when I get up I can hardly walk sometimes. A lot of clots… I am scared to go to the hospital because I don’t know how I will be able to pay. Even just to hear what caused the death of my baby. I am just thinking ‘was I stressed?’, ‘was I not eating well?’, ‘was it a time I slipped on the stairs?’ Or was it a medical problem? I don’t know.”
Duty of Care
A new Maternity Action report “Duty of Care” highlights the contradictions facing staff.
The Nursing & Midwifery Council Code requires all nurses and midwives to “respect and uphold people’s human rights” and “act as an advocate for the vulnerable, challenging poor practice and discriminatory attitudes and behaviour relating to their care.”
One specialist midwife told of a refused asylum seeker with HIV who declined to continue antenatal care after receiving a large bill. She was considering delivering the baby at home without professional help.
Although HIV treatment is exempt from charging, maternity care is not. But without proper treatment, a woman may risk transmitting HIV to her baby during labour or afterwards. Further, HIV-positive women will be charged a higher price for their maternity care by virtue of their HIV diagnosis.
Her specialist midwife said “It’s horrific, she doesn’t trust anyone any more. She’s very negative regarding her pregnancy.
She felt that the midwife in the booking was quite judgemental. Unfortunately it’s left a feeling that people along the way are quite judgemental in considering why she’s not married.”
The midwife managed to access additional funding to continue the woman’s antenatal care at home
Reporting Debt in a City of Sanctuary
In July, the Yorkshire Evening Post published a letter from KONP Co-chair and retired Consultant Dr John Puntis, noting the ironic contrast of “Leeds as a city of sanctuary and its great tradition of welcoming immigrants” with “the ‘hostile environment’ which now requires Leeds Teaching Hospitals NHS Trust (LTHT) to charge vulnerable and impoverished migrants for healthcare”.
Dr Puntis also asked the Trust “Why does LTHT report patients with debts over £500 to the Home Office when such reporting is not mandatory?”
The Trust replied: “Although not a mandatory requirement, compliance is expected by NHS Improvement. The Trust has an obligation to take all steps available to recover the cost of providing care to those not eligible for NHS treatment and prevent the loss of public funds.”
The issues are being raised within Unite, whose branch chair also chairs the Trust staff-side committee.
Royal Liverpool Hospital
In November 2018 KONP Merseyside and the Save Liverpool Women’s Hospital campaign organised a Patients Not Passports conference, supported by Unite North West, Liverpool TUC, Unite branches and Garston & Halewood CLP. Speakers included Maternity Action, Docs Not Cops, Medact, South Yorkshire Migration and Asylum Action Group, Greater Manchester Law Centre, and These Walls Must Fall, with support from Refugee Women Connect and Asylum Link Merseyside.
Consultant Microbiologist Dr Jonathan Folb from the Royal Liverpool hospital attended and began raising the issue with Junior Doctors and other Consultants.
In January, 60 medics and public health academics met at the Medical School, with input from Docs Not Cops and KONP. Medics expressed outrage at the charges and their implementation in the hospital. KONP later learned that the charges to “overseas visitors” in 2018-19 amounted to 0.12% of total patient care income, and only 0.04% was actually paid, negating any economic argument for the regime.
In a survey of Junior Doctors and Consultants, over 100 of each group responded, and over 90%
of each stated opposition to the charges. The Joint staff-side, with unions representing all other NHS staff in the hospital, is also supportive.
A campaign statement inviting signatures was placed on the Medact website.
The local GP surgery dealing with asylum seekers and refugees wrote to the campaign, ccing the Trust Interim CEO and Chair, “[To] restrict access to necessary healthcare is, in the opinion of the Board of PC24, neither in the spirit of the NHS nor the ethos of Liverpool as an asylum city. As an organisation, Primary Care 24 fully supports your campaign and will help in any way we can to bring this practice to an end.”
In July, medics convened a Grand Round (to discuss issues and individual cases), with participation from the GP surgery and migrant support group “Refugee Women Connect”.
The Acting Medical Director invited Consultants to redraft the Trust policy. It turned out there is currently no agreed policy, only a draft, but the charging regime is operating.
This offer posed a difficult question. Medics had to decide whether accepting it would make them complicit in a regime they completely oppose.
On the other hand, patients are being charged, posters are up and women wearing a headscarf have been asked for their passport at A&E.
The Overseas Visitor Team become involved before clinical teams have had time to properly assess urgency or clinical exemptions. The OVT read and append the clinical notes, and interview relatives while patients are undergoing treatment, pulling in staff to interpret.
Over the summer, medics decided to redraft the policy. On 23 Oct, the second anniversary of the introduction of upfront charges, a campaign meeting attended by Consultants, senior staff, Junior Doctors from the Royal, Aintree and Warrington hospitals, the Walton Centre, medical students and a former interpreter endorsed this approach and agreed to submit an updated version for negotiation with Liverpool University Hospitals NHS Foundation Trust (merger of Royal and Aintree).
The draft opens by referring to “First Do No Harm”, the GMC Duties of a Doctor, the Duty of Care covering all staff and the Trust itself, and the Caldicott Principles.
It acknowledges the concerns expressed by staff and endorses calls from the British Medical Association, Academy of Medical Royal Colleges, and the Royal College of Midwives, for the regulations to be repealed or suspended pending a full and independent review into the impact of charging on individual and public health.
The draft policy is introduced as an interim measure to mitigate harm as far as possible while remaining within the 2015 and 2017 Regulations. It sets out procedures to identify exemptions, with charges as the last resort and without a target in the Business Plan. No charges, publicity or inquiries will occur in the Emergency Department or Sexual Health (GUM).
Only clinicians will access clinical data. Limited nonclinical data will only be shared with the Home Office on an individual basis with patient consent, in line with Caldicott, after other attempts
to find exemptions have failed.
Patients will have access to advocates and interpreters on request, and appeal rights. The Trust will not use external debt recovery agencies and will not report debt to the Home Office. The draft sets out roles and responsibilities for each staff group including the Overseas Visitor Team. It requires the Trust Board to monitor the policy’s full impact on Patient Safety, Equality and Diversity and on the health of patients who present, or could otherwise be expected to present, to the Trust.
Major problems will remain until the law is repealed. But campaigners and hospital staff hope that Liverpool University Hospitals will choose to stand alongside the BMA and others in calling for a change in the law, while protecting patients and staff in the interim.
The BMA Mersey Junior Doctors Committee wrote to the campaign in July, expressing support in line with BMA policy (below), and concluding:
We also as a local committee support your call to Royal Liverpool University Hospital to make a public statement acknowledging the concerns of its staff, and encourage them to support the calls from BMA and other key stakeholders to abandon charging, and to take immediate interim measures to reduce harm to vulnerable individuals, ensuring the NHS is free for all at the point of delivery.
BMA and Royal Colleges
The BMA Annual Representative Meeting (ARM) in June overwhelmingly adopted Motion 42 from Tower Hamlets Division:
That this meeting notes that in a pilot to check eligibility for free NHS Care only 1/180 people were deemed ineligible and:-
i) this meeting believes that it is not cost effective to monitor eligibility for NHS Care;
ii) this meeting calls for the policy of charging migrants for NHS care to be abandoned and for the NHS to be free for all at the point of delivery;
iii) that this meeting believes that the overseas visitors charging regulations of 2011 threaten
the founding principles of the NHS and that the regulations should be scrapped.
The Academy of Medical Royal Colleges called for “the suspension of the NHS charging regulations
pending a full and independent review of the impact on both individual and public health” and “a clear separation of roles between immigration enforcement activities and the provision of healthcare”.
The Royal College of Midwives Chief Executive Gill Walton, introducing the Maternity Action “Duty of Care” report, stated:
“We believe that maternity care should be exempt from NHS charging altogether to protect and promote maternal and newborn health. The current charging regime needs to be suspended until the government can prove this policy is not doing any harm and jeopardising our shared ambition to make England the safest place in the world to have a baby.”
Labour
Labour Party Conference agreed NHS Composite 2 which includes:
“Conference supports health workers’ duty of care to migrants and opposes migrant charges. Labour will repeal Sections 38 and 39 of the Immigration Act 2014 and subsequent regulations which implement migrant charges.”
A motion from Labour Women’s Conference was adopted overwhelmingly.
“Annual Women’s Conference deplores the 2017 introduction of NHS charging regulations requiring undocumented and destitute migrant and refugee women to pay ‘up front’ charges for antenatal and maternity care.
… “We resolve to:
“call on the Secretary of State for Health and Social Care and the Government to rescind the Regulations – and meanwhile suspend them pending research on their impact
“call on the Shadow Secretary of State for Health and Social Care to express Labour’s opposition to charging and agree to rescind the policy under a Labour government”
Dear Reader,
If you like our content please support our campaigning journalism to protect health care for all.
Our goal is to inform people, hold our politicians to account and help to build change through evidence based ideas.
Everyone should have access to comprehensive healthcare, but our NHS needs support. You can help us to continue to counter bad policy, battle neglect of the NHS and correct dangerous mis-infomation.
Supporters of the NHS are crucial in sustaining our health service and with your help we will be able to engage more people in securing its future.
Please donate to help support our campaigning NHS research and journalism.