The Government’s plans to train teachers to spot the signs of mental illness in their pupils are “little more than a sticking plaster”, says the National Educational Union.
Any genuine strategy to tackle mental health problems in young people should include efforts to reduce poverty and inequality and reverse NHS and school budget cuts, suggested Dr Mary Bousted, Joint General Secretary of the NEU.
Responding to Theresa May’s announcement that the government will improve mental health training opportunities for teachers she said:
“Schools need strong pastoral systems, but teachers cannot cover for the cuts to mental health specialists. Recognising the early signs is important but timely routes to appropriate professional treatment is essential.
At the moment referrals lead to long waiting times – children and young people should not have to threaten or attempt suicide before accessing CAMHS”.
Social workers and healthcare professionals are also set to be given more opportunities to access better mental health training as part of new policy to improve early intervention and prevention announced by the outgoing Prime Minister. NHS staff will have access to suicide prevention training. This latest policy announcement echoes that of Jeremy Hunt’s promise while he was heath secretary in 2017 to put a mental health lead in all schools by 2025.
Yet, chronic cuts to mental health services, alongside the impact of austerity policies on schools, families and local authorities since 2010 have resulted in a mental health care crisis within the NHS which successive health secretaries have repeatedly noted, but failed to meaningfully tackle.
A young people’s crisis
Though the well documented crisis in mental health care affects people of all ages, mental health services for young people in particular have failed to keep up with demand. This is in part due to an increase in demand in recent decades as admissions to hospital for self-harm have almost doubled since 1997, and self-reported mental health conditions among young people have increased six-fold in England since 1995.
While health care professionals must be at the forefront of treatment, teachers have long felt under-resourced in this area.
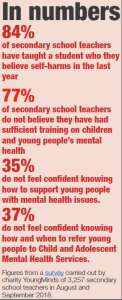
A recent survey of teachers by charity YoungMinds highlighted 84 per cent of secondary school teachers have taught a pupil they believe self-harms, and 77 per cent of teachers did not feel they had sufficient training on children and young people’s mental health.
Nearly half of pupils do turn to teachers for help when struggling with their mental health, figures from NHS Digital in 2018 reveal.
The NEU had been calling on the Government to put children’s wellbeing at the centre of education policy for some time, Dr Bousted continued, but “the ‘exam factory’ culture of testing, driven from Whitehall, is one significant cause of anxiety and low self-esteem among young people,” she explained.
Staffing slashed
Yet, while demand for mental health services is high and rising, cuts and austerity have meant that there are even fewer services than ever before for children and young adults to access. Over 20,000 roles were unfilled in the mental health sector in September 2018, with up to 2,000 staff leaving a month, figures from the Department of Health and Social Care showed. This is despite Hunt’s promise in 2017 to deliver 19,000 more mental health staff by 2021.
Nurse numbers have been particularly hard hit, with the scrapping of the bursary, uncertainty over Brexit and increasingly challenging working conditions all playing a role in the current 14.3 per cent vacancy rate for mental health nursing roles across England.
This represents a 13 per cent reduction in the total number of mental health nurses across all settings since 2010. A 19 per cent reduction in the total number of school nurses in England as well, doesn’t help.
Why is there a crisis in our mental health services?
Mental Health: a stronghold of private provision
Support our NHS campaigning journalism
Catherine Gamble, Royal College of Nursing Professional Lead for Mental Health Nursing, points out that teachers already identify and support pupils with mental health issues, but notes: “It is vital, however, that there is sustained investment in mental health nursing to ensure those in need have access to the full range of treatments once mental health issues are identified”.
This week the College said an additional £1 billion funding for nurses education was required at a minimum, if the Government was to recruit enough nurses to realise its NHS Long Term Plan.
Reduction in capacity
Even if there were enough staff to deal with the number of young people who need mental health services, it is unlikely the system has enough capacity to take them. The number of beds for mental health patients in England fell 30 per cent since 2009.
An overhaul of children’s mental health services announced by Hunt in 2017 promised to slash waiting times for CAHMs to just four weeks from referral. Yet, an HSJ investigation last year showed hundreds of children were waiting more than a year, and over half of children referred to CAHMs were forced to wait 18 weeks.
What young people need
Early intervention for mental health is important, but similar to all other areas of health, it is useless if it is not the first step towards appropriate treatment.
Nick Harrop, Campaigns Manager at YoungMinds who have been campaigning for better early intervention for young people said: “We know from the young people we work with how hard it can be to access mental health support, and there is still a long way to go before help is available to every young person who reaches out.
“With rising demand, prevention and early intervention should be genuine priorities, and we need to see greater investment in community support beyond the NHS, so that young people can get the help they need when problems first emerge.”
Dear Reader,
If you like our content please support our campaigning journalism to protect health care for all.
Our goal is to inform people, hold our politicians to account and help to build change through evidence based ideas.
Everyone should have access to comprehensive healthcare, but our NHS needs support. You can help us to continue to counter bad policy, battle neglect of the NHS and correct dangerous mis-infomation.
Supporters of the NHS are crucial in sustaining our health service and with your help we will be able to engage more people in securing its future.
Please donate to help support our campaigning NHS research and journalism.



